
Recommendation-Specific Supportive Text
- If well tolerated, beta blockers should be continued in patients who are currently receiving them for longitudinal reasons, particularly when longitudinal treatment is provided according to GDMT(guideline-directed management and therapy), such as for MI. Multiple observational studies support the benefits of continuing beta blockers in patients who are undergoing surgery and who are on these agents for longitudinal indications.
- 특별한 indication이 있어서 beta blocker를 사용하는 경우(ex. MI)에는 수술 기간에도 BB의 사용을 권장한다.
- In the absence of conclusive RCTs, the expert opinion of this writing committee is that control of BP to levels recommended by the present guideline (BP <130/80 mm Hg) or other target levels specified for a particular individual is reasonable before undertaking major elective procedures in either the inpatient or outpatient setting. If the patient is unable to take oral medications, it is reasonable to use intravenous medications as necessary to control BP. Special consideration of parenteral therapy usually occurs for patients taking clonidine or beta blockers because of the risk of stopping these medications acutely. Withdrawal syndromes, accompanied by sympathetic discharge and acute hypertension, can occur on cessation of these agents.
- 결정적인 RCT가 없는 상황에서, BP 조절은 현재 가이드라인에 따른 BP 값 혹은 개인별 target BP값을 맞추도록 노력한다. 만약 경구 복용이 어려운 상황이라면 IV 고혈압약제로 BP를 조절하도록 한다.
- Clonidine or BB를 사용하는 환자에서 갑작스러운 약물 중단은 위험할 수 있으니 주의깊은 모니터링이 필요하다. 특히나 금단 현상(교감신경 실조 및 급성 고혈압을 동반)이 발생할 수 있으니 주의해야 한다.
- Data on the potential risk and benefit of ACE inhibitors in the perioperative setting are limited to observational analyses, and this area is controversial. Recent evidence from a large cohort study demonstrates that patients who stopped their ACE inhibitors or ARBs 24 hours before noncardiac surgery were less likely to suffer the primary composite outcome (all-cause death, stroke, or myocardial injury) and intraoperative hypotension than were those continuing these medications until surgery.
- 수술 전후의 ACEI 약제에서 득과 실에 대한 데이터는 자료가 부족하긴 하지만 대규모 코호트 연구의 최근 증거는 심장 수술 24시간 전에 ACE 억제제 또는 ARB를 중단한 환자가 수술 전까지 이러한 약물을 지속하는 환자보다 일차 임상 결과(all-cause death, stroke or myocardial injury)와 수술 중 저혈압을 겪을 가능성이 적다는 것을 보여준다.
- JNC 6 noted conflicting evidence for patients with DBP >110 mm Hg and recommended delay of surgery for gradual reduction in DBP before proceeding with surgery. In a systematic review and meta-analysis of 30 observational studies, preoperative hypertension was associated with a 35% increase in cardiovascular complications. An increase in complications, including dysrhythmias, myocardial ischemia or infarction, neurological complications, and renal failure, has been reported in patients with DBP ≥110 mm Hg immediately before surgery. In contrast, patients with DBP <110 mm Hg do not appear to be at significantly increased risk.The relationship of systolic hypertension to surgical risk is less certain. Among patients undergoing carotid endarterectomy, increased risk of postoperative hypertension and neurological defects were observed, and an increased risk of CVD morbidity after coronary artery bypass graft surgery has been observed in patients with isolated systolic hypertension. During induction of anesthesia for surgery, sympathetic action can result in a 20– to 30–mm Hg increase in BP and a 15- to 20-bpm increase in heart rate among patients with normal BP. Exaggerated responses may occur in patients with poorly treated or untreated hypertension by as much as 90 mm Hg and 40 bpm. With further anesthesia, the accompanying inhibition of the sympathetic nervous system and loss of baroreceptor control may result in intraoperative hypotension. Lability in BP appears more likely in patients with poorly controlled hypertension, whereas studies have observed that patients with controlled hypertension respond similarly to those who are normotensive. Early work indicated that patients with severe hypertension (SBP >210 mm Hg and DBP >105 mm Hg) had exaggerated responses in BP during the induction of anesthesia.
- JNC 6에서는 DBP > 110 mgHg 환자에 대해 DBP control 이후의 수술을 권고했다. 여러 관찰 연구와 메타 분석 등에서 수술 전 고혈압은 수술 후 심혈관 합병증을 35%나 증가시켰다. 관련 합병증으로는 부정맥, 심근경색, 신경학적 합병증 및 신부전 등도 포함된다. 수술을위한 마취 중 교감신경을 자극하여 BP가 20~30 mmHg 상승되고 심박수가 15-20 bpm 증가될 수 있다. 이를 control 하기 위한 추가 마취제의 투여는 교감신경계 억제와 혈압수용체(baroreceptor)의 상실로 인해 수술 중 저혈압이 야기될 수 있다. BP의 안정성은 잘 조절되지 않는 고혈압 환자에게서 더 많이 나타나는 반면, 잘 조절되는 고혈압 환자의 경우 정상 혈압 환자와 유사하게 BP가 조절된다.
- Although few studies describe risks of withdrawing beta blockers in the perioperative time period, longstanding evidence from other settings suggests that abrupt withdrawal of long-term beta blockers is harmful. There are fewer data to describe whether short-term (1 to 2 days) perioperative use of beta blockers, followed by rapid discontinuation, is harmful.
- 수술 기간 동안 BB를 중단하였을 때 위험을 설명한 연구는 거의 없지만 다른 환경(조건)에서 장기간 BB를 갑자기 중단하였을 때 해롭다는 연구의 증거는 다양하다. BB의 단기(1-2일)간 수술 전 갑작스런 중단이 해로운지 여부를 설명해주는 근거는 적다.
- The 2014 ACC/AHA perioperative guideline specifically recommㅇends against starting beta blockers on the day of surgery in beta-blocker–naive patients, particularly at high initial doses, in long-acting form, and if there are no plans for dose titration or monitoring for adverse events. Data from the POISE (Perioperative Ischemic Evaluation) study demonstrate the risk of initiating long-acting beta blockers on the day of surgery.
- 2014 ACC/AHA perioperative guideline에서 수술 끝난 당일 BB를 사용하지 않는 환자에서 BB를 사용하지 말 것을 권고하며 특히나 고용량의 초기 용량, 장기간 작용 제제, 부작용에 대한 모니터링이 없는 경우라면 더더욱 말이다. POISE(Perioperative ischemic Evaluation) 연구에서 수술 당일날 장기간 작용 BB의 사용에 대한 위험이 밝혀졌다.
장기간 작용 BB(long acting BB) : metoprolol
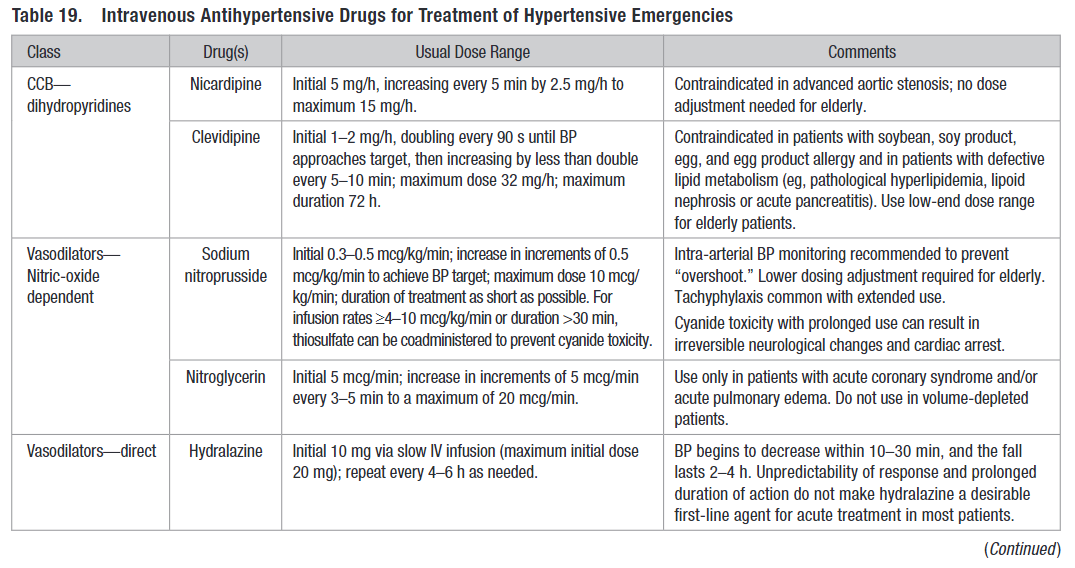
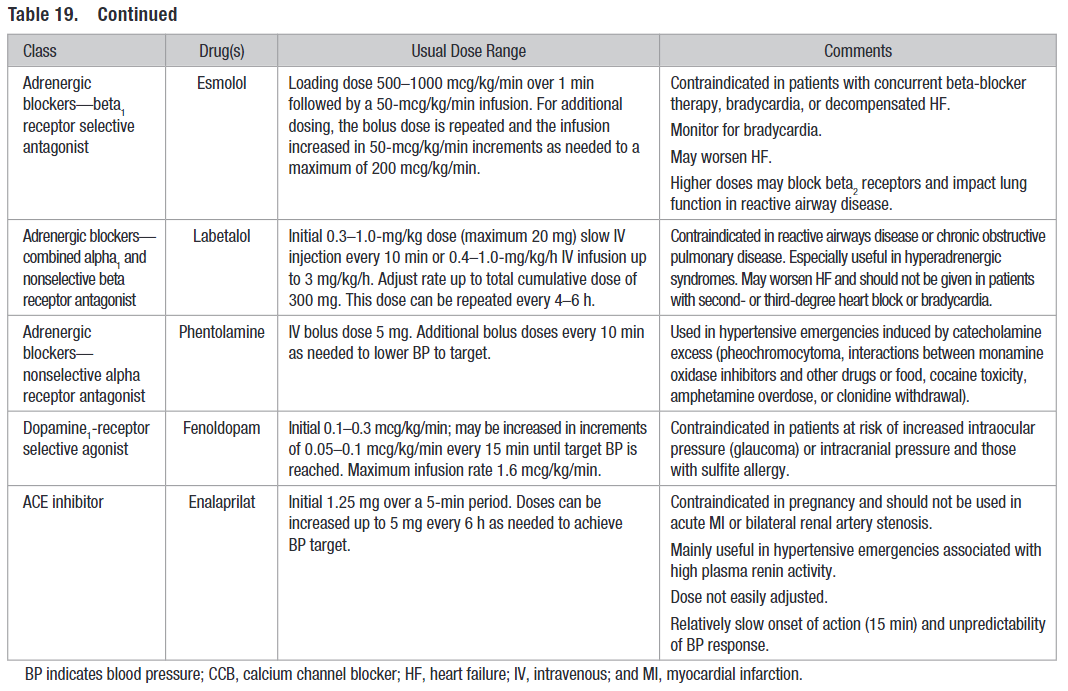
- Several antihypertensive agents in a variety of pharmacological classes are available for the treatment of hypertensive emergencies.
- hypertensive emergencies의 치료를 위해 다양한 고혈압 약제를 사용할 수 있다(table 19, 20 참조)

reference:
1) Whelton, Paul K., et al. "2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines." Journal of the American College of Cardiology 71.19 (2018): e127-e248.
728x90
'🤹♂️ 카테고리별 약물 > 심혈관' 카테고리의 다른 글
| 고혈압 신약 : 저항성 고혈압 치료, baxdrostat, Aldosterone synthase inhibitor, 알도스테론 합성효소 저해제 (1) | 2023.02.06 |
|---|---|
| TRANSFORM-HF trial : loop계 이뇨제, Toresemide vs Furosemide (0) | 2023.02.01 |
| 혈압 변동성 큰 환자에서 amlodipine, CCB, BP variability (0) | 2023.01.26 |
| 골절 환자에서 정맥혈전증 예방 요법 : Thromboprophylaxis, Aspirin, Low-Molecular-Weight Heparin (0) | 2023.01.24 |
| Thiazide 이뇨제 차이 : chlorthalidone vs hydrochlorothiazide (0) | 2023.01.04 |


댓글