일차성 고알도스테론혈증
- 알도스테론은 부신 피질에서 생성되는 호르몬으로 신장에 작용하여 수분/전해질/혈압 조절을 관장함
- 한쪽 또는 양측 부신에서 알도스테론이 과잉 생성되는 질환
- 고알도스테론혈증 상태에서 염분의 흡수와 소변을 통한 칼륨 방출을 증가시켜 고혈압을 유발

Saline infusion test
- 앙와위 자세로 적어도 1시간 유지
- 0.9% saline infusion 2L over 4hr
- renin, aldosterone, cortisol, potassium을 0, 2, 4시간 마다 측정
- cut off value plasma aldosterone (1 ng/dL=10pg/mL)
- >10 ng/dL: highly diagnostic
- <5 ng/dL: unlikely(=정상)
Captopril challange test
- 앙와위 자세로 적어도 30분간 안정
- captopril 50 mg 복용 후 0, 60, 90 분 마다 측정
- cut off value
- ARR >20 or PAC >12 ng/dL: 양성
Fludrocortisone salt loading test
- 4일 동안 fludrocortisone 0.1 mg q6h + 케이콘틴 정과 같은 서방형 potassium chloride q6h(혈중 K수치를 4 mmol/L 유지하기 위함)
- 혈중 K 농도 1일 4회 측정
- high sodium dite + sodium chloride (urinary sodium ecretion rate of at least 3 mmol/kg)
- 4일 째, 오전 7시(8시) & 오전 10시 plasma cortisol 측정, 오전 10시 PAC, renin 측정
* 4일동안 f/u이 필요하므로 잘 사용하지 않을 것으로 예상됨

* 플로리네프 정 특징 (반드시 냉장보관해야하는가?)
- 저장방법 2-8도 보관
- 설정된 저장방법에서 벗어난 실온(25℃)에서 최대 30일까지 보관이 가능하다. 실온 보관 후 사용되지 않은 정제를 다새 냉장보관하지 않고 폐기한다.
특징: 저칼륨혈증 & 조절되지 않는 고혈압
- 약제 내성(치료 불응성) 고혈압
- systo-diastolic hypertension(BP >150/100 mmHg)
- 자연적인 or 이뇨제 유도 저칼륨혈증
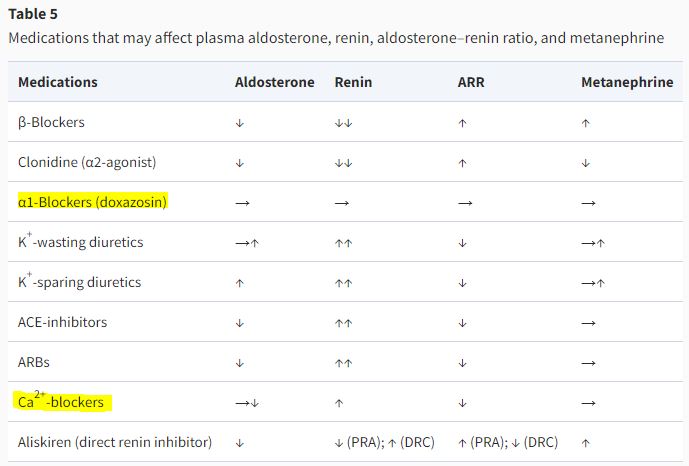
실험값에 영향을 미치는 요인 & 복용 가능한 약제
복용중인 약제에 따라 ARR에 영향을 끼칠 수 있음
따라서 일차성 고알도스테론을 의심 하 진단검사를 시행할 때 환자의 복용 약제를 리뷰해야 함
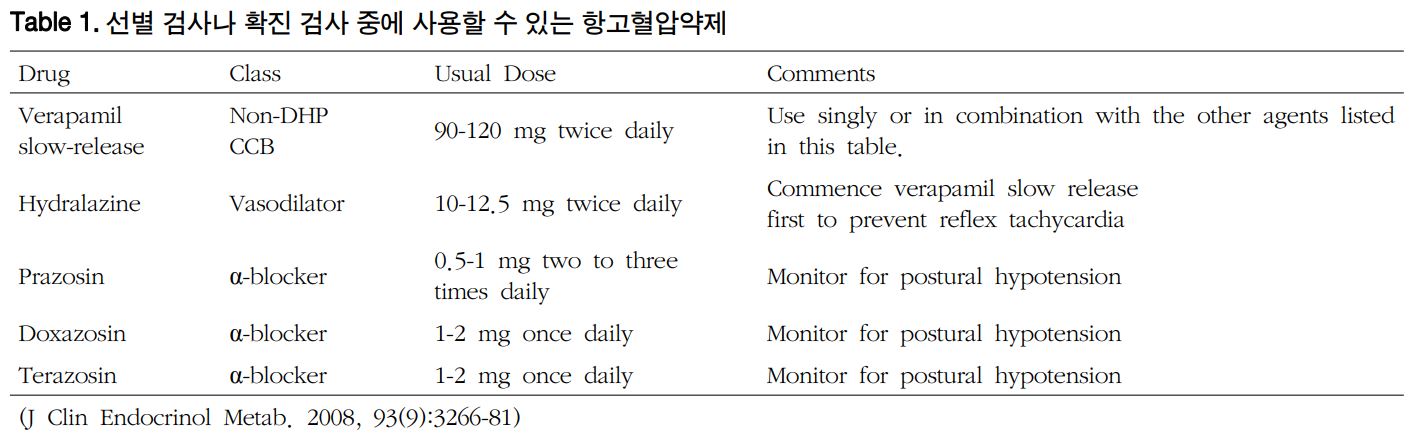
- possible BP medication: verapamil-SR, hydralazine, praxosin, doxazosin
치료: 수술 요법 vs 약물요법
수술요법 - unilateral laparoscopic adrenalectomy(with proven unilateral dz)
약물요법 - mineralocorticoid receptor antagonist(MRA) in combination with other 고혈압약제: BAH(bilateral adrenal hyperplasia) or not suitble for surgery
- Spironolactone: MR 비선택적이므로 여성형 유방, 발기부전, 생리 불순 등의 부작용 있음, the progestational and antiandrogenic side effects(항안드로겐성) of the non-specific aldosterone receptor antagonist
- Epleronone: 국내 X, MR에 더 특이적이므로 상대적으로 부작용이 덜할 것으로 예상. 하지만 비급여 약제임(2022.03.06 기준)
spironolactone vs epleronone
The aim of this prospective, randomised, open-label, blinded-end point study was to compare the efficacy and safety of eplerenone versus spironolactone in patients with bilateral idiopathic hyperaldosteronism (IHA). After a 2-week washout period, 34 patients with IHA were assigned to receive either spironolactone 25 mg b.i.d. (n = 17) or eplerenone 25 mg b.i.d. (n = 17) for 24 weeks. If the patients' blood pressure (BP) was not < 140/90 mmHg, the doses were gradually increased up to 400 mg for spironolactone and 200 mg for eplerenone. If the patients' BP remained uncontrolled, a daily dose of hydrochlorothiazide 12.5 mg was added at week 16. The primary outcome was the percentage of patients with BP < 140/90 mmHg at 16 weeks (i.e., with aldosterone antagonist monotherapy). The patients' BP was normalised in 13 out of 17 (76.5%) and 14 out of 17 (82.4%) patients in the spironolactone and eplerenone groups, respectively (p = 1.00). Systolic BP decreased more rapidly with eplerenone. Serum potassium levels were normalised (> 3.5 mmol/l) in all patients at 4 weeks. Mild hyperkalaemia was observed in two patients receiving 400 mg of spironolactone and in three patients receiving 150 mg of eplerenone. Two patients presented with bilateral painful gynaecomastia at the end of week 16 while receiving 400 mg of spironolactone. Switching spironolactone to 150 mg of eplerenone daily resulted in resolution of gynaecomastia and also maintained BP control. At the end of the study, 19 patients were on eplerenone and 15 were on spironolactone. However, this did not affect the primary end point, because the switch from spironolactone to eplerenone (in two patients) occurred at the end of week 16. It was concluded that eplerenone was as effective as spironolactone in reducing BP in patients with IHA. The risk of mild hyperkalaemia was similar with both drugs.
reference:
1) Rimoldi, Stefano F., Urs Scherrer, and Franz H. Messerli. "Secondary arterial hypertension: when, who, and how to screen?." European heart journal 35.19 (2014): 1245-1254.
2) 김상완. "Essentials of Primary Care: 내분비-대사 (제이드); 일차성 알도스테론혈증의 재발견." 대한내과학회 춘계학술발표논문집 2015 (2015): 207-210.
3) 약학정보원
4) Brown, Nancy J. "Eplerenone: cardiovascular protection." Circulation 107.19 (2003): 2512-2518.
5) Karagiannis, Asterios, et al. "Spironolactone versus eplerenone for the treatment of idiopathic hyperaldosteronism." Expert Opinion on Pharmacotherapy 9.4 (2008): 509-515.
'🤹♂️ 카테고리별 약물 > 내분비' 카테고리의 다른 글
| 인슐린 똑똑하게 사용하기, 자가혈당 측정 방법, 인슐린 용량 조절 방법 (2) | 2023.10.16 |
|---|---|
| 고지혈증약(statin계)-당뇨 유발, 스타틴 약물, 당뇨 위험도 증가 (3) | 2023.08.22 |
| 조영제에 의한 신독성 예방, 조영제-metformin 중단 시기 & 중단 기준 (0) | 2022.02.11 |
| 부신 호르몬 검사 시 영향을 주는 약제, cortisol, ACTH, PAC/PRA ratio, 카테콜아민 (0) | 2021.12.27 |
| Glucocorticoid, steroid, WBC 증가, leukocytosis, 백혈구 증가증 (0) | 2021.12.26 |


댓글